June is Men’s Health Month, a good time to talk about the health of those men in your life. Below, Dr. Daren Wu, Chief Medical Officer of Open Door Family Medical Center, answers questions about men’s health and the reluctance many men seem to have in seeking health care.
1. Have you found that men are less likely to visit their doctor or follow screening protocols (unless pushed by their family)?
My wife will be the first to say that unless she makes the medical appointment for me, I am very unlikely to see a doctor! This may sound familiar to many men. My reluctance to seek out health care is very common among men. There are stark gender differences in health care utilization, not only in the United States, but across the world. Men simply are less likely to seek medical attention, and this tendency cuts across all ethnicities and racial groups.
Moreover, while men are much less likely to have preventive care – such as for physicals and recommended care like immunizations and cancer screenings – they also are less likely to seek help even when they are aware of problems or are experiencing health-related symptoms, including pain and disabling problems.
2. If so, how do you convince them to change their ways?
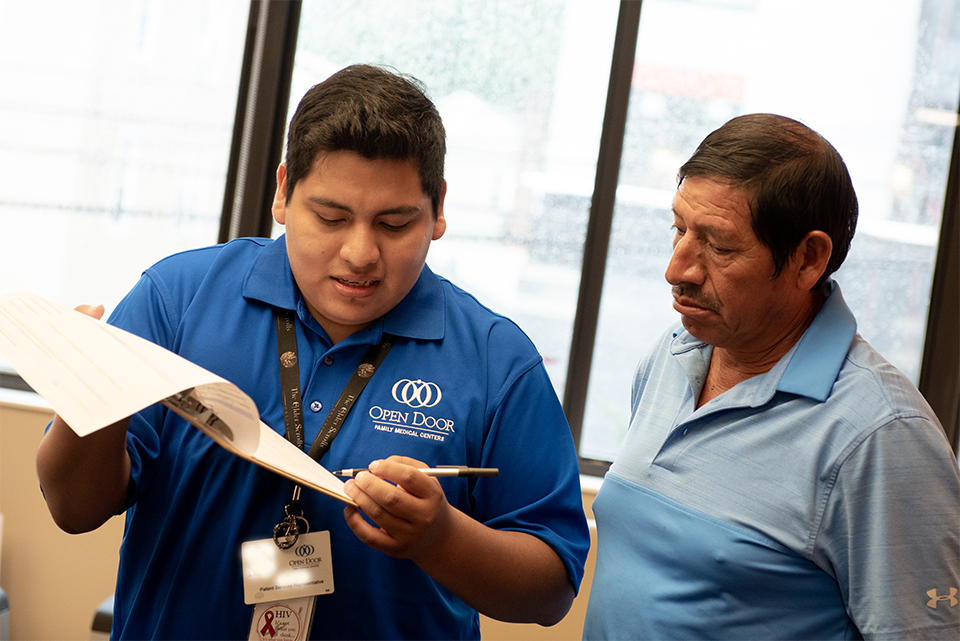
All patients benefit from having a trusted relationship with health care providers, and I have found that men seem to really need to trust a clinician prior to opening up about their concerns and problems.
A strategy that my colleagues and I often employ is to frame good health as not just important for the man himself to have, but for him to continue providing for his partner and children. Some men may not be motivated to take care of themselves as much as they feel the need to be able to keep being a provider for their families. Sometimes men can be convinced to take care of themselves if recommendations are put in the context of staying healthy so that they are able to take care of their families.
3. What are the more important screening protocols men need to follow?
The biggest contributor to mortality — by far, even in this age of COVID-19 – has been and remains heart disease. According to the latest data from the American Heart Association, one out of every two American adults now has hypertension, or high blood pressure, and this is the main cause of heart disease. Men need to be screened for the factors driving heart disease – high blood pressure, high cholesterol, high blood sugar (diabetes), tobacco use, sedentary lifestyles – and treated if these apply to them.
There are several cancers that can be found earlier and have higher likelihood of successful treatment, if screened according to guidelines. Colon cancer screening is one of the most important recommendations to review with men, starting at age 45. Colon cancer is relatively straightforward to detect and to treat with excellent prognosis, when found early. There is an excellent lung cancer screening option, using annual low-dose CT imaging of the chest, for those who have a significant smoking history, starting at age 50.
Men should also be aware of the need to consider screening for prostate cancer. Prostate cancer is the most common cancer for men, excluding skin cancer. In fact, at least 10 percent of men will eventually develop prostate cancer. It is also the second leading cause of cancer-related deaths for men, after lung cancer. Prostate cancer screening is not a universal recommendation, but a discussion on the pros and cons of prostate screening, starting at age 55, is a very good idea.
Crucially, men need to be better screened for mental health. Gun violence is all over the news, and the perpetrators are almost always males, frequently with difficult upbringings or challenges that simply were not addressed, or were under-evaluated and/or under-treated. Suicide is also a major problem among males, and in recent years the rise in suicides among middle-aged men has been very concerning. Across all nationalities and ethnicities, men tend to have greater barriers towards opening up and being willing to talk about their stressors, anxieties, and depression symptoms, which makes it harder to diagnose and adequately treat these conditions in men.
4. Why do you think men are more reluctant than women to see a doctor?
In part, men begin interacting with health care later than women, who due to gynecological, birth control, and pregnancy-related needs are more acquainted with the health care system and so continue to utilize health care with greater frequency.
5. Do you think this hesitancy is reflected in one’s health/longevity (any studies that indicate this)?
Yes, and multiple studies prove that. Even accounting for gender disparities that skew greater resources and protocols being developed based on men’s health, and less on women’s health, male longevity across all demographic groups and nations around the world lag compared to that of women, and that is not accounted or explained by biological factors.
6. Anecdotally, do you remember how you convinced a male patient that he had to start following screening protocol (or simply see their doctor)?
Absolutely, and this is why I allude to the need to engage men in their own health needs by emphasizing their importance to their families.
One patient, let us call him Jack, has been struggling with excessive alcohol use for many years. Like many men and women who have a problem with overusing alcohol, there are underlying mental health concerns that trigger his drinking habit, but certainly there is a physiologic chemical addiction as well.
The way I got through to Jack on being more proactive in adhering to alcohol treatment, after many attempts at discussing why it is so potentially dangerous for him to continue drinking as much as he does – liver cirrhosis, esophageal and stomach cancer, heart disease, and so on – was by framing how devastated his wife and daughter would be if he were unable to continue working in construction and painting. He is the sole breadwinner in his household. Aside from the stress of navigating through painful and difficult health complications from excess alcohol use, he could very easily devastate his family’s financial well-being if no longer able to be a provider for them. That got him to be more adherent with his treatment plan. Alcohol treatment is always challenging but given that he now has a clearer vision of what is at stake – not just his own health, but the well-being of his loved ones – he is more motivated to take better care of himself.